Pseudomyxoma Peritonei (PMP)
A rare tumour in which the abdominal cavity is filled with a ‘jelly-like’ substance
What is Pseudomyxoma Peritonei?
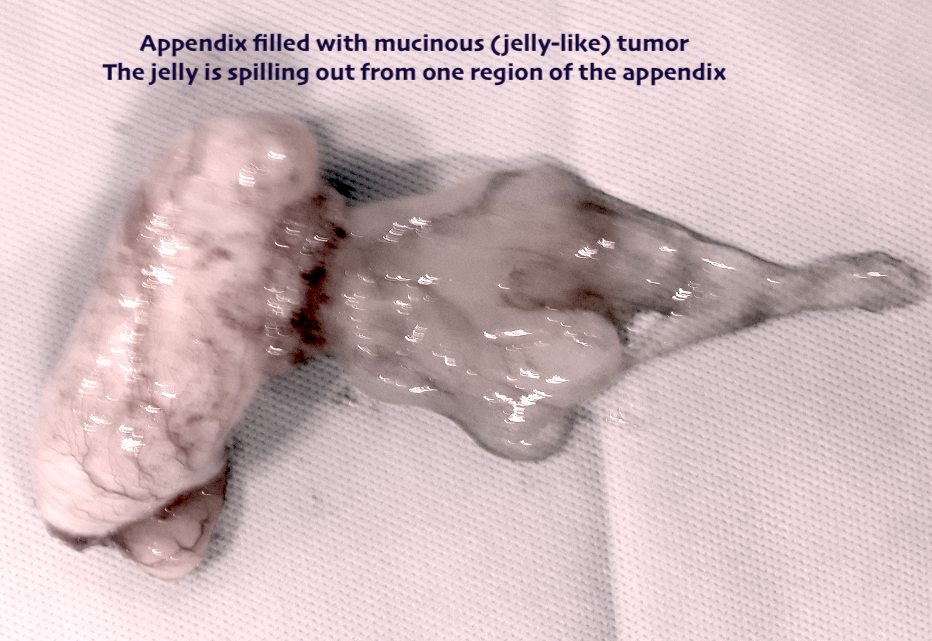
Pseudomyxoma Peritonei also known as PMP or jelly belly, is a rare condition characterized by the presence of mucin-producing tumors (mucin is a jelly like substance) in the abdominal cavity. It can originate from many parts of the body, but the most common source of PMP is appendiceal (appendix) cancer.
If left untreated, the tumor can grow in size leading to excessive collection of mucin. This produces discomfort due compression of the organs in the abdominal cavity. The resultant swelling also compresses the diaphragm leading to difficulty in breathing. It may cause intestinal blockage.
The age at diagnosis ranges from late teens to later stages of life, with most of the individuals being diagnosed in their 40′s and 50′s. It is generally thought that there is no genetic (hereditary) link to PMP. It affects men and women as well. PMP is often initially misdiagnosed as ovarian cancer in women and often initially diagnosed as a hernia, especially in men.
PMP is a rare tumour and the odds of being diagnosed with PMP is about 1 in a million. However, due to prior misdiagnosis or misclassification, it is more common now. Risk factors that might predispose an individual to develop PMP are still unknown.
What are the Causes?
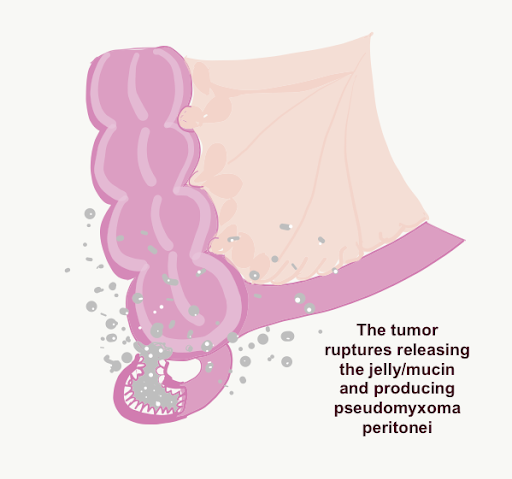
There are a number of theories on the origins of PMP, but there is no known underlying cause. It is generally accepted that appendix cancer is the most common source of the tumors that cause PMP. Cells from a mucinous tumor in the appendix leak into the abdominal cavity and implant on the peritoneum or other abdominal organs. These tumors replicate and produce a mucinous byproduct that spreads throughout the abdomen.
The other common sites of origin of PMP are the ovary, stomach, colon, pancreas and other abdominal organs.
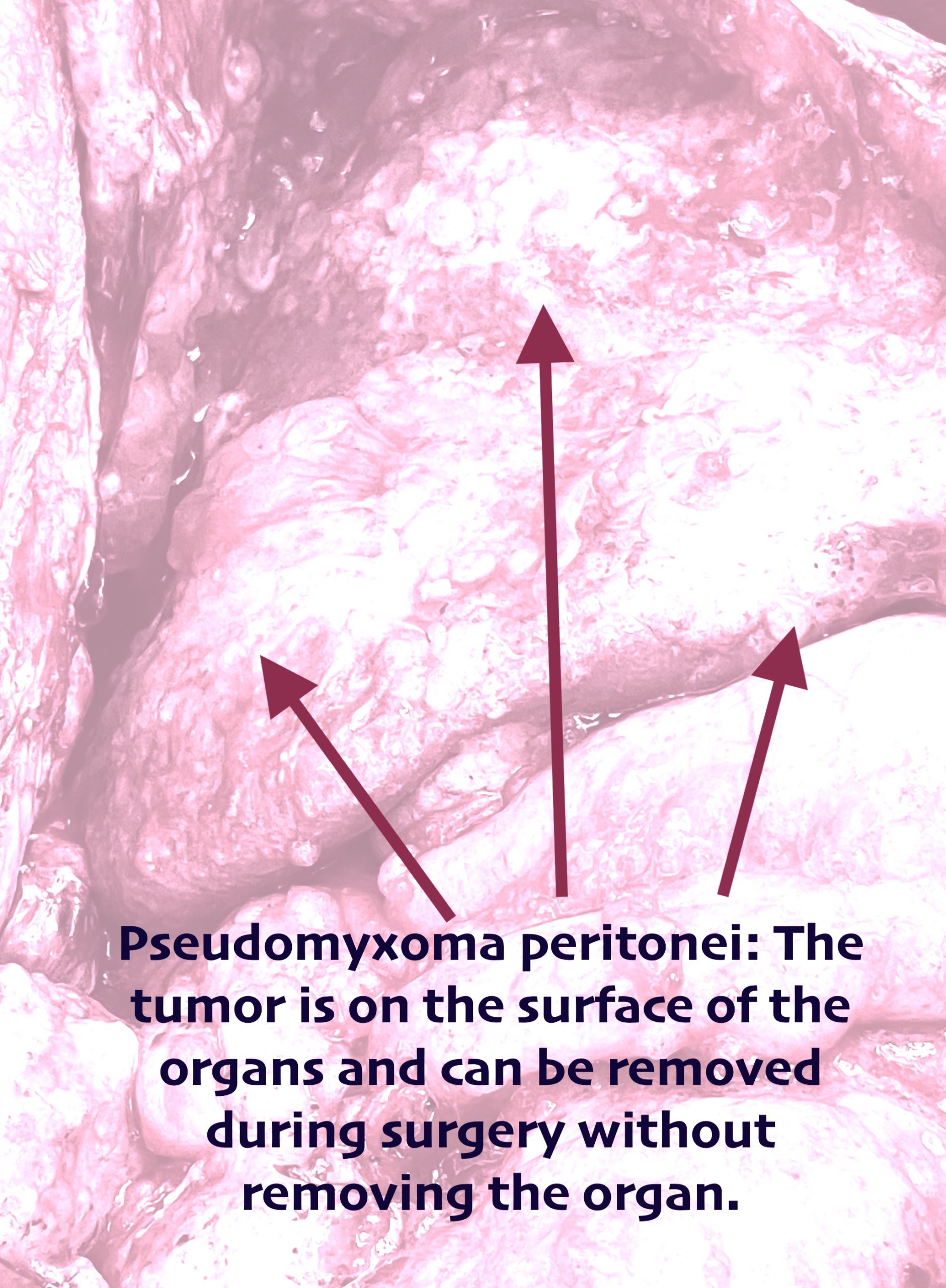
PMP has a tendency to remain confined to the peritoneal cavity for a prolonged period. It keeps growing in size within the peritoneal cavity. It can cover the surface of the organs from outside and interfere with their normal function at a very late stage. It may also spread to the pleural cavity (the space around the lungs).
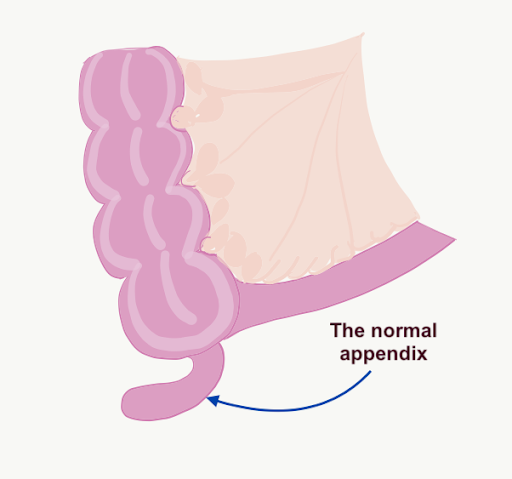
Pictorial Representation
The normal appendix
Mucinous tumor in the appendix leading to swelling of the appendix
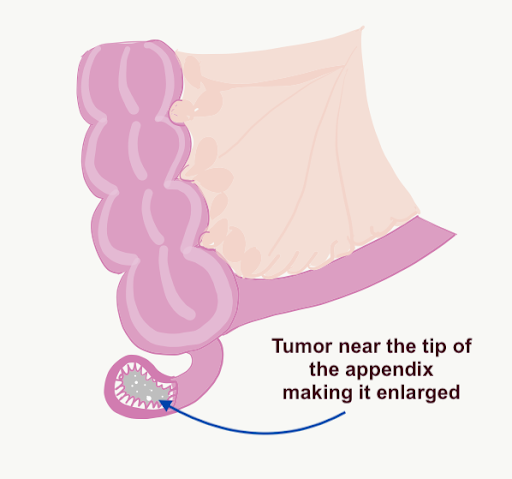
The appendix ruptures and releases the mucinous tumor which implants all over the peritoneal cavity resulting in pseudomyxoma peritonei or jelly belly
What are the Symptoms?
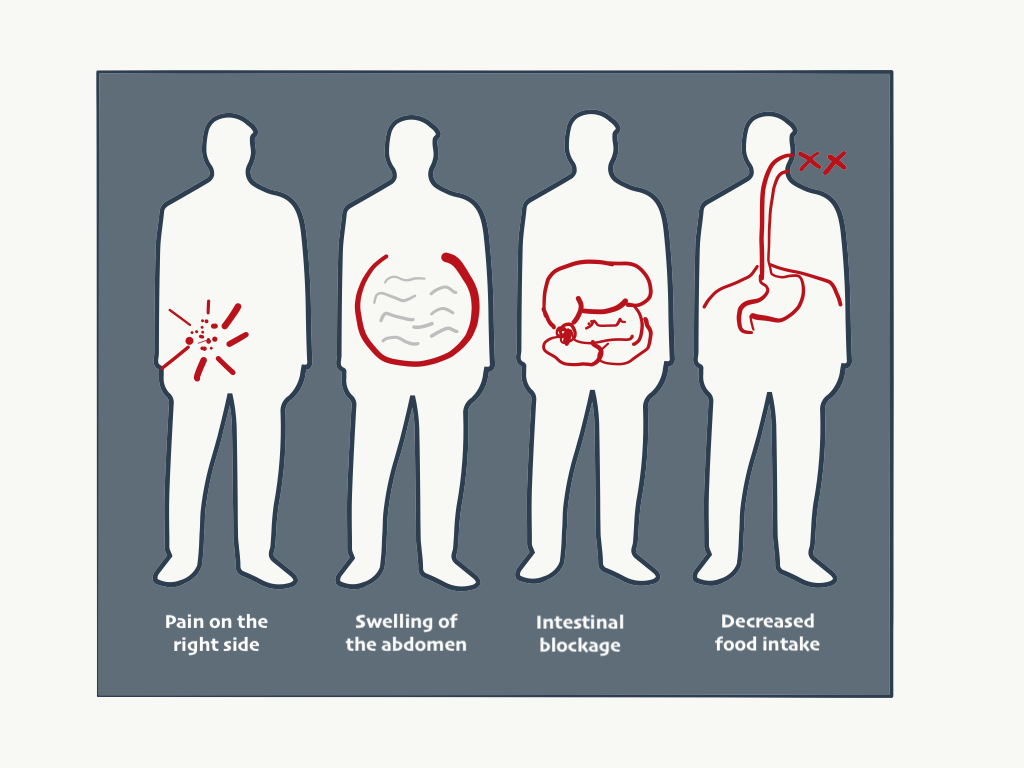
Many patients lack clearly defined symptoms, until the disease reaches a relatively advanced stage.
Here are some of the most common symptoms of PMP:
• Bloating
• Increased abdominal girth or swelling of the abdomen
• Pain/discomfort in the abdominal region (dull ache or sharp pains similar to appendicitis)
• Hernia symptoms
• In women, symptoms of an ovarian cyst or tumor
• Ascites (fluid) buildup in the abdominal cavity
How is PMP Diagnosed?
For many patients, PMP is discovered during an unrelated surgical procedure. At that time, the surgeon observes the mucinous tumors or “studding” on the peritoneum or on other abdominal organs. A specialist may be able to diagnose the tumor from certain tell-tale signs of the tumor in CT scans and Ultrasonography.
The following diagnostic tests are commonly used in diagnosing PMP:
• CT scan of the chest, abdomen & pelvis:CT scans have some tell-tale signs of pseudomyxoma that can lead to the diagnosis. Though this is true in most of the cases, CT scans are still not the perfect pictures. This is because the visible signs of tumor are not present in a CT scan of some patients. CT scans also require the judgement of a radiologist who can interpret the scan to identify the signs of PMP.
• Diagnostic laparoscopy:Laparoscopy allows direct inspection of the tumor and enables a biopsy. This helps in determining the extent of disease and knowing the grade of the tumor which is useful for deciding the course of treatment.
• Blood tests (tumor markers):Some tumor markers in the blood have been shown to be indicative of PMP activity, particularly CEA, CA-125, and CA 19-9. Unfortunately, tumor markers are not accurate indicators for everyone. Some patients will have no elevation in their tumor markers, despite having extensive tumours.
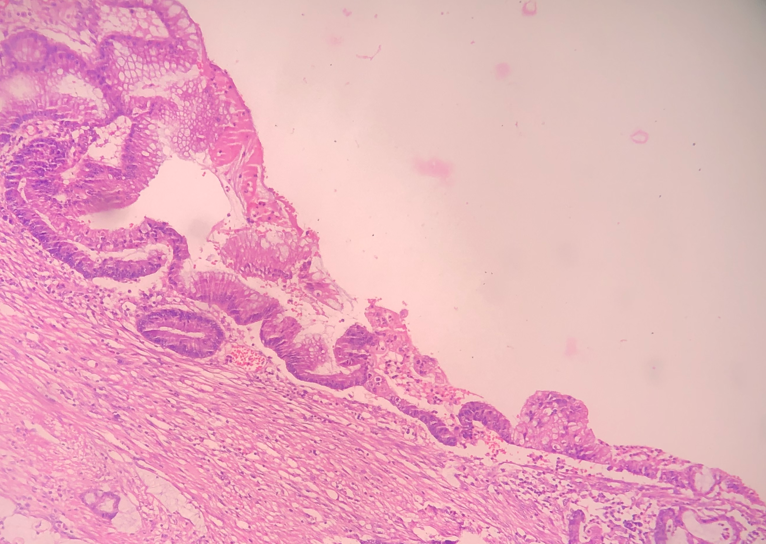
• Biopsy:Tissue from the mucinous deposits or the primary tumor if seen, may be taken to prove the diagnosis before starting treatment. It is also important to know the grade of the tumor. Low grade tumors have a more favourable outcome as compared to high grade tumors. However, many times, there is excessive jelly with only few cells which may make it difficult to determine the type of tumor (high grade or low grade) on the biopsy sample alone. Secondly, when only jelly-like substances come out during biopsy, some pathologists may misdiagnose it as a non-cancerous or benign condition.
Mostly pathologists are not able to recognize the tumor correctly, resulting in an incorrect diagnosis. However, in the last two decades, the awareness has increased among the medical community and most reputed and experienced pathologists are able to make a correct diagnosis. When in doubt, doctors seek a second opinion from another doctor who is more experienced with these tumors.

The Treatment
The “standard of care” for the treatment of PMP is generally a combination therapy that consists of specialized cytoreductive surgery (CRS), followed by localized application of heated intraperitoneal chemotherapy (HIPEC). It removes all of the tumors and affected tissues. The key to success is the surgical acumen, if some tumor is left behind, a recurrence is unavoidable.
For most patients PMP is considered treatable, but not curable. However, there are a growing number of individuals who have undergone cytoreductive surgery and HIPEC and experienced many years of disease-free survival. These individuals are those patients whose disease was detected early and with favourable pathology (low grade tumors). For others, the treatment relieves them from some or all of the symptoms that affect their quality of life.
A team of doctors work on each case, and this team includes a PMP specialist accompanied by another experienced surgeon, a team of anaesthetists, intensive care specialists, medical oncologists, trained nurses, physiotherapists and dieticians.
Currently, no consensus is there in the medical community on the use of systemic chemotherapy and/or radiation in treating PMP. Some individuals appear to benefit from systemic chemotherapy while others do not. However, neither chemotherapy nor radiation have proven to be curative for PMP. For high grade tumors, the use of intravenous or systemic chemotherapy can help in prolonging life if the tumor cannot be completely removed or if it recurs.
